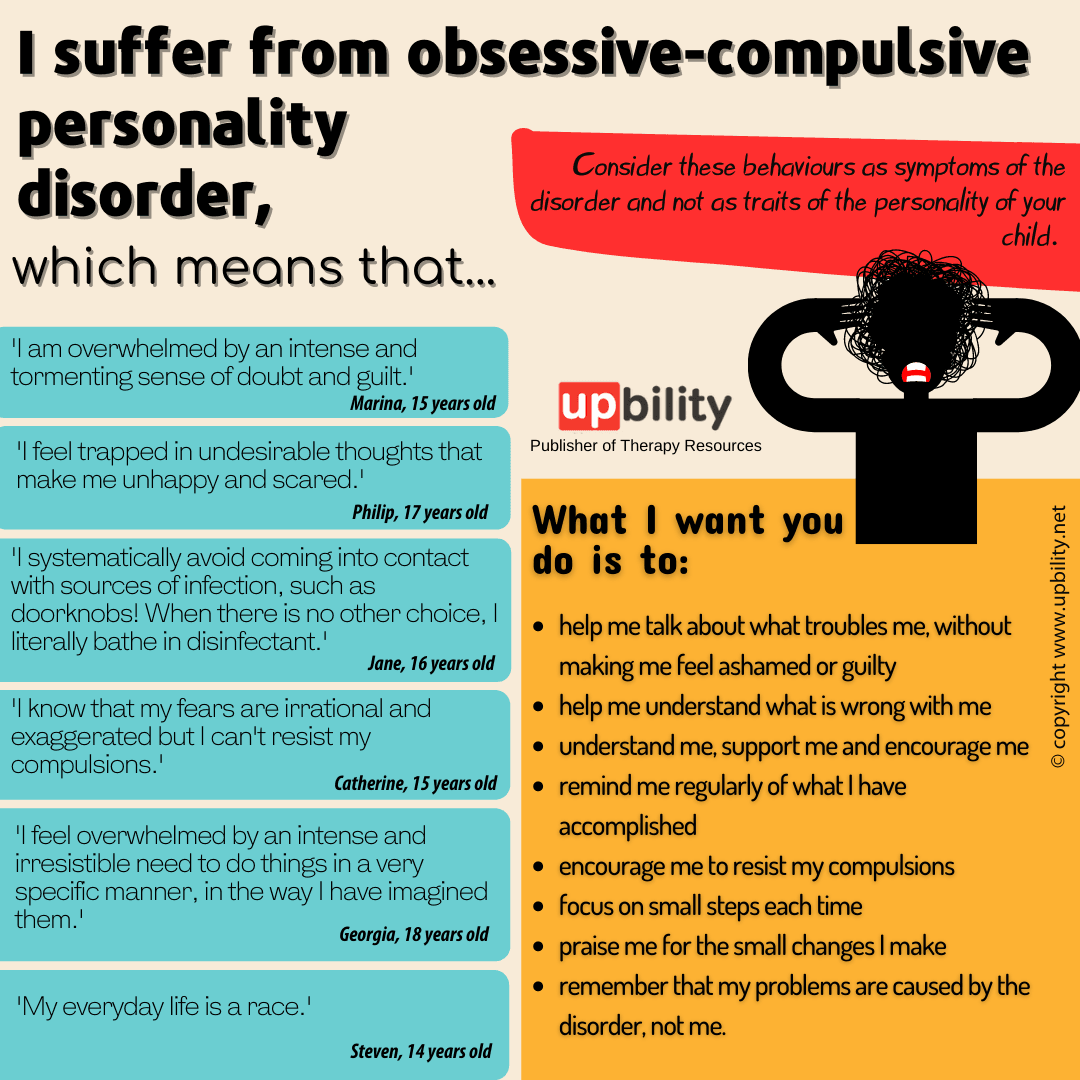
I suffer from obsessive-compulsive personality disorder
What is OCD?
Obsessive-compulsive disorder (OCD) is a mental disorder that involves obsessions (compulsions) and compulsions. It is one of the most common mental illnesses affecting children and adolescents. It is reported to occur in 1-3% of people. It is the fourth most common mental illness after phobias, substance abuse and major depression.

Compulsions are repeated visible or mental acts, usually of a ritualistic nature. The person performs them in response to an ideology or according to rules that must be strictly obeyed. They are intended to counteract the obsessions and reduce the anxiety they cause.
In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), obsessive-compulsive disorder (OCD) is classified as an anxiety disorder. The criteria for diagnosing OCD in the DSM-5 include:
Presence of obsessions, compulsions, or both: obsessions are defined as recurrent and persistent thoughts, impulses, or images that are intrusive and unwanted and cause anxiety or distress. Compulsions are defined as repetitive behaviours or mental acts that the person feels driven to perform in response to an obsession or according to rigid rules.
Obsessions or compulsions are time-consuming or cause significant distress or harm: The symptoms of the disorder must occupy a significant amount of time (more than one hour per day) or cause significant distress or harm to social, occupational or other functioning.
The obsessions or compulsions are not due to another medical or psychiatric condition: The symptoms of OCD are not best explained by another medical or psychiatric condition.
The obsessions or compulsions are not related to substance use or medication: OCD symptoms are not best explained by substance use or medication.
Identification: The DSM-5 also includes determinations for the presence of insight (whether the individual recognizes that his or her obsessions or compulsions are excessive or irrational) and severity of the disorder (based on the level of interference with functioning).
Obsessive-compulsive disorder ideations:
- fear of infection (I will be infected by something I touched)
- perfectionism (excessive preoccupation with precision, order and symmetry)
- fear of causing harm to myself or another person
- doubts and fear of something bad happening (the kitchen eye, the unlocked door)
- Preconceived notions (lucky and unlucky numbers, if I don't do this...something bad will happen, etc.)
- unwanted thoughts of sexual, violent or blasphemous content (mostly teenagers)
OCD compulsions:
- Frequent and excessive washing and/or cleaning, usually in a ritualistic manner
- Frequent and excessive rechecking (that he hasn't forgotten something)
- Tidying and precision of objects in a certain way that is always the same.
- Frequent and persistent reassurances (Nothing will happen to me..)
- Repeating the same actions (rereading or rewriting something,)
- Mental compulsions (prayer, counting)
- Excessive worry about trivial things and trivialities
- Putting objects in order or rearranging them until he feels a sense that everything is "okay"
- Accumulating items, thinking that they may need them in the future
- Sequence of specific behaviours
- Verbal compulsions
Causes of OCD
OCD has a neurobiological basis, with studies showing that the brain functions differently in people with the disorder. An abnormality, or imbalance in neurotransmitters, is involved in the disorder.
Genetic factors:
There is evidence that OCD may have a genetic component. Studies have shown that people with first-degree relatives who have OCD are at greater risk of developing the disorder themselves.
Brain structure and function:
Obsessive compulsive disorder-obsessive compulsive disorder ocd has been associated with alterations in certain brain regions and neurotransmitter systems involved in the regulation of mood, anxiety, and behavior.
Environmental factors:
Traumatic events, abuse or stress can trigger or worsen the symptoms of OCD in some individuals.
Behavioral conditioning:
Some individuals may develop OCD behaviors as a way of coping with anxiety or stress, which over time becomes a repetitive and compulsive behavior.
Cognitive factors:
Obsessive compulsive disorder (OCD) may be associated with specific thought patterns, such as a tendency to overestimate the likelihood of harm or "all or nothing" thinking.
What might be the warning signs of OCD?
The child/adolescent may:
- Be very late in completing a task even in simple activities
- Ask frequent and persistent questions about the health of family members
- Worries excessively about trivial things and unimportant details
- Reacts extremely to trivial things
- Has difficulty and/or delays going to bed to complete tasks
- Changes his eating habits
- Displays strong indecisiveness
- He/she has great difficulty in going about his/her daily life
- Spends an unreasonable amount of time on daily routines, such as personal hygiene, eating or dressing
- Repeating the same actions over and over again
- Persistently asks for reassurances and does not reassure easily
- He is a perfectionist, gets angry and easily loses his temper if he does not get something perfect
- His daily routine is very difficult to manage
- He tries to hide his strange behaviour, "disappearing" for a long time in the toilet or in his room
- Becomes extremely angry and upset when interrupted during a routine or daily activity
Obsessive compulsive disorder (OCD) can affect every aspect of a person's life, leading to significant distress, anxiety and disruption of daily functioning.
The symptoms of OCD can manifest in a variety of ways, including excessive cleaning and washing, checking and rechecking, repetitive behaviors, intrusive thoughts, avoidance behaviors, excessive worrying and perfectionism.
These symptoms can lead to prolonged and disruptive behaviours, interfering with daily activities and social relationships. For example, spending excessive time and effort on cleaning and disinfecting can affect performance at work or school or limit one's ability to participate in social activities.
Repetitive behaviours, such as hitting or touching objects or arranging objects, can be time-consuming and interfere with productivity or concentration. Persistent thoughts and excessive worry can cause significant anxiety and distress, leading to avoidance behaviour and limiting the person's ability to participate in activities they enjoy.
Perfectionism can lead to rigid thinking and difficulty adapting to changes or unexpected situations, which can affect social relationships and work or school performance.
It is important to note that not everyone with OCD experiences all of these symptoms and the severity of symptoms can vary greatly between individuals. However, when untreated, OCD can significantly affect a person's quality of life, leading to social isolation, anxiety and depression.
How does OCD affect children and adolescents?
OCD can make everyday life very stressful for children. Rituals usually take a long time and children are often late for school or activities. This often leads to tensions or conflicts within the family. Children cannot enjoy time with friends or have fun when compulsions take up all their free time. At school, obsessions and rituals such as checking, crossing off and re-doing assignments affect attention and concentration, completion of assignments and school attendance. Older children and adolescents do not understand what is happening to them, they worry and work hard to hide their compulsions. Their days are busy and they often break their sleep schedules in order to complete their responsibilities. Consequently, they sleep late and are tired during the day. All this stress affects their emotions (sadness, anger, tantrums).
How does OCD affect the family?
The family often suffers when a child presents with OCD. Initially, parents may be confused or frustrated by their child's odd behaviours. They may become frightened when their child becomes upset and seems unable to stop the compulsions.
Children may push their families to engage in OCD in many, different ways: They often seek reassurance by repeatedly asking their parents the same questions and demanding answers each time. They may need help from parents and siblings to complete their rituals. They may insist parents and siblings follow their compulsions. They may become very angry if they do not get their way. All this is very stressful for the family, who feel that they cannot relax and that life at home is very tense. Parents may feel that they have to change the family routine or give in to the child's demands to prevent the child's anger and anxiety. It is natural to go through many different emotions, such as fear, frustration, anger, guilt and sadness. They often worry about whether their child will recover and what their future will be like.
Can OCD be treated in children and adolescents?
Yes, OCD can be treated in children and adolescents. In fact, early diagnosis and treatment can help prevent the condition from interfering with a child's social and academic development. Treatment of OCD in children and adolescents often involves a combination of medication and psychotherapy.
Medication: Selective serotonin reuptake inhibitors (SSRIs) are a type of medication commonly used to treat OCD in children and adolescents. These medications can help reduce anxiety and obsessions and compulsions.
Cognitive-behavioral therapy (CBT): CBT is a type of psychotherapy that can help children and adolescents learn how to manage and reduce the symptoms of OCD. Exposure and response prevention therapy (ERP), a specific type of CBT, involves gradually exposing the child to situations or objects that trigger the symptoms of OCD and teaching the child to resist performing compulsive behaviors.
Family therapy: OCD can affect the entire family, and family therapy can help families understand the condition and learn ways to support their child's treatment.
Cognitive performance
Obsessive-compulsive disorder (OCD) can have an impact on cognitive performance. Research suggests that people with OCD may experience difficulties in certain cognitive functions, including:
Attention: symptoms of the disorder can be highly distracting and demanding, making it difficult for individuals to focus on tasks or filter irrelevant information.
Working memory: Working memory refers to the ability to retain and manipulate information in the mind for a short period of time. People with OCD may have difficulties with working memory, which can affect their ability to plan and organize tasks.
Decision-making: symptoms of OCD can lead to excessive chatter and indecision, making it difficult for individuals to make decisions or take action.
Cognitive flexibility: Cognitive flexibility refers to the ability to change one's thinking or behavior in response to changing demands or situations. Individuals with OCD may have difficulties with cognitive flexibility, which can affect their ability to adapt to change or respond to unexpected situations.
However, it is important to note that not all people with OCD experience cognitive difficulties and the extent of these difficulties can vary widely between individuals. Treatment for OCD, such as cognitive-behavioural therapy (CBT) and medication, can help reduce symptoms and improve cognitive function.
What is Cognitive-Behavioural Psychotherapy (CBT) and how does it work?
Cognitive-behavioural therapy (CBT) is a type of psychotherapy that has been shown to be effective in the treatment of obsessive-compulsive disorder (OCD). CBT for OCD OCD usually includes two main components: exposure and response prevention (ERP) and cognitive therapy.
Exposure and response prevention (ERP): ERP is a type of behavioral therapy that involves gradually exposing the person with OCD to situations or objects that trigger their obsessions while preventing them from engaging in compulsive behaviors.
The goal is to help the person learn to tolerate the anxiety associated with their obsessions without resorting to compulsions. Over time, the individual learns that he or she can cope with his or her obsessions without performing compulsive behaviors.
Cognitive therapy: This component of CBT focuses on identifying and changing the negative or unrealistic beliefs and thoughts that may be contributing to the symptoms of OCD. For example, a person with OCD infection may have the belief that all germs are harmful and can cause illness. Cognitive therapy can help him or her challenge this belief and learn to think more realistically about the real danger of germs.
CBT for OCD is usually conducted in 12-20 weekly sessions, and the therapist may also assign homework exercises to reinforce the skills learned in therapy. Research has shown that CBT can be just as effective as medication in treating OCD, and many people show long-term improvement with this treatment.
It is important to work with a mental health professional with experience in treating OCD using CBT. Treatment plans should be tailored to the individual's needs and for some people a combination of medication and psychotherapy may be used.
Medication in children and adolescents with OCD
Selective serotonin reuptake inhibitors (SSRIs) are a type of medication commonly used to treat obsessive-compulsive disorder (OCD) in children and adolescents. These medications work by increasing levels of the neurotransmitter serotonin in the brain, which can help reduce anxiety and obsessions and compulsions.
The US Food and Drug Administration (FDA) has approved several SSRIs for the treatment of OCD in children and adolescents, including fluoxetine (Prozac), sertraline (Zoloft) and fluvoxamine (Luvox). These drugs are generally well tolerated, but some potential side effects include nausea, insomnia and decreased appetite.
When prescribing medications for children and adolescents with OCD, healthcare providers usually start with a low dose and gradually increase it over time. They will also monitor the person closely for any side effects or changes in symptoms.
I think my child may have OCD, what should I do?
If you suspect your child may have obsessive-compulsive disorder (OCD), it is important to seek professional help. Here are some steps you can take:
Talk to your child's health care provider: Start by scheduling an appointment with your child's healthcare provider, such as his or her pediatrician. He or she can help you assess your child's symptoms and refer you to a mental health professional who has experience treating OCD.
Consult a mental health professional: A mental health professional, such as a psychologist or psychiatrist, can conduct a thorough evaluation to determine if your child has OCD and develop an appropriate treatment plan.
Learn about OCD. This can help you to better understand your child's experience and support your child in their treatment.
Be supportive: Children with OCD can experience significant stress and distress and it is important to provide emotional support and reassurance. Encourage your child to talk about their feelings and experiences and let them know that you are there to help them.
Encourage therapy: OCD can be effectively treated with a combination of medication and psychotherapy. Encourage your child to participate in treatment and give them positive reinforcement for their progress.
Aliki Kassotaki - Speech and Language Therapist MSc, BSc
Original content from the Upbility writing team. This article, in whole or in part, may not be republished without attribution to the publisher.
Copyright Upbility 2022