Symptoms, Treatment, and Prevention Tips
If there is one group of bacteria that has made its mark on human health, it’s Streptococcus. From causing simple sore throats to life-threatening conditions, these microbial culprits are not to be underestimated. But what exactly are these bacteria, and how do they wreak such havoc? Let’s dive in and find out.
Key Takeaways
-
Streptococcus is a Gram-positive bacteria responsible for mild to severe illnesses.
-
Symptoms of streptococcal infections include sore throat, fever, and swollen lymph nodes in the neck.
-
Prevention measures against Streptococcus involve regular handwashing and vaccination for high risk populations.
Unveiling Streptococcus: A Microbial Culprit
Streptococcus, a group of Gram-positive bacteria, is responsible for an array of diseases that vary in severity. The spectrum of diseases caused by these bacteria ranges from mild illnesses such as strep throat to severe conditions, including necrotizing fasciitis and streptococcal toxic shock syndrome. It is important to understand when and how streptococcal disease occur in order to effectively prevent and treat these infections.
Interestingly, these bacteria also have a significant role in industrial and dairy processes.
The Basics of Streptococcus Bacteria
Streptococcus bacteria are:
-
Nonmotile
-
Nonsporulating cocci
-
Found in pairs or chains
-
Characterized by the absence of the catalase enzyme
-
Characterized by the presence of structural proteins such as M proteins, which facilitate attachment to host epithelial cells
These bacteria are commonly found on the skin and throat and can cause a skin infection in humans.
Severe gas infection can develop invasive gas disease when the bacteria infiltrate further into the body, potentially leading to invasive disease. It is crucial to understand the factors that contribute to when invasive gas disease occur in order to develop effective prevention and treatment strategies.
Diseases Caused by Streptococcus
Streptococcal infections can lead to a wide range of illnesses, including:
-
Asymptomatic carriage
-
Mild infections such as strep throat
-
Skin infections such as impetigo
-
Invasive diseases such as necrotizing fasciitis and streptococcal toxic shock syndrome (STSS)
The most severe manifestations of invasive group A streptococcal diseases are necrotizing fasciitis and STSS.
Severe illnesses can be attributed to certain strains of group A streptococcus, which produce toxins and enzymes leading to shock, organ damage, and tissue destruction.
Signs and Symptoms of Streptococcal Diseases
Streptococcal infections present with a variety of symptoms that depend on the specific disease. Common indications and manifestations encompass:
-
sore throat
-
difficulty swallowing
-
headache
-
fever
-
red and swollen tonsils
-
white patches on the tonsils
-
swollen lymph nodes in the neck
Recognizing Strep Throat
Characterized by a severe sore throat, discomfort when swallowing, and fever, strep throat is a common streptococcal infection. Other symptoms include inflamed and enlarged tonsils and sensitive lymph nodes at the front of the neck. The symptoms generally become apparent 2 to 5 days after exposure to the bacteria.
Identifying Severe Streptococcal Infections
Manifestations of severe streptococcal infections may include bloodstream infections (bacteremia) and conditions like scarlet fever, which result in a rash, sore throat, and high fever. The rash associated with scarlet fever typically initiates on the face or neck and then extends to the chest, trunk, arms, and legs. It is characterized by a red and bumpy appearance and may exhibit a sandpaper-like texture.
How Streptococcus Spreads and Infects
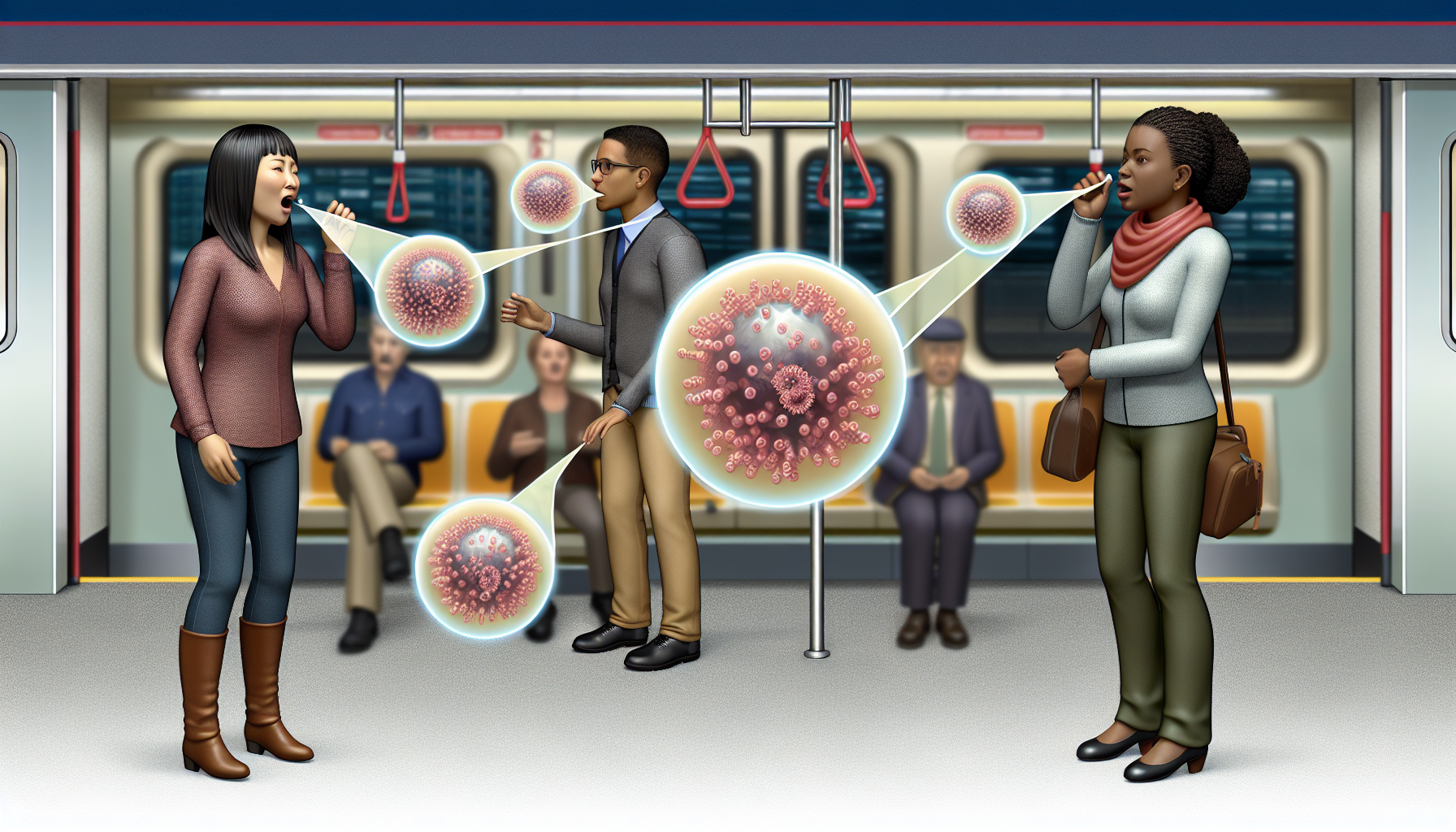
Streptococcal bacteria are spread through diverse methods including coughing or sneezing, contact with infected wounds or sores, and during vaginal delivery. Additionally, asymptomatic carriers, who display no signs of infection, can still transmit the bacteria to others.
Invasive group A streptococcal infections arise when the body’s defenses are penetrated by the bacteria, often through open wounds or compromised immunity from health conditions.
Transmission Pathways
Streptococcus can spread through:
-
Respiratory droplets when an infected individual coughs or sneezes, thereby releasing the bacteria into the air. Subsequently, these droplets can be inhaled by others, facilitating the transmission of the bacteria.
-
Direct contact with discharges from the nose and throat of infected individuals.
-
Contact with infected wounds.
Streptococcus bacteria have the potential to remain viable on a dry surface for a period ranging from 3 days to 6.5 months, thereby indicating the potential for transmission through contact with contaminated surfaces.
Risk Factors for Developing Invasive GAS Disease
Certain risk factors can increase the susceptibility to developing invasive GAS disease. These include pre-existing health conditions such as diabetes and cancer, undergoing kidney dialysis, and having close contact with someone infected with GAS disease. All these conditions can lead to changes in the immune system, potentially reducing the body’s capacity to combat infections.
Diagnosing Streptococcal Infections

Accurate diagnosis of streptococcal infections is crucial for proper treatment. Diagnosis involves laboratory tests, including:
-
Bacitracin test
-
Lancefield antigen A test
-
Strep A test
-
Throat culture
-
Rapid antigen detection testing
-
ASO test
Diagnosis also relies on cultures obtained from clinical specimens, which may include sputum, blood, or cerebrospinal fluid in some cases.
Laboratory Tests for Accurate Diagnosis
Detection of Streptococcus in a throat culture involves the following steps:
-
Swab the back of the throat with a sterile cotton swab.
-
Place the swab in a culture medium.
-
Send the swab to a laboratory for analysis.
-
Results can typically be obtained within 24 to 48 hours.
In addition, rapid antigen detection tests (RADTs) used for diagnosing Streptococcus function by identifying particular antigens produced by the bacteria. These tests are capable of delivering rapid results in approximately five to ten minutes, rendering them appropriate for point-of-care diagnosis.
Importance of Early Detection
Numerous advantages are offered by early detection of streptococcal infections, including timely treatment, prevention of complications, and reduced transmission of the infection. Early detection plays a crucial role in treatment by enabling the swift initiation of antibiotics, which are the primary course of treatment for streptococcal infections.
It aids in preventing complications, reducing symptom duration, and implementing appropriate isolation measures for disease control, containing the spread of infection.
Battling Streptococcus: Antibiotic Treatment and Challenges

The primary treatment for streptococcal infections is antibiotics. Penicillin is the preferred medication for both mild and severe illnesses caused by Streptococcus, including invasive group A streptococcal disease. However, the issue of antibiotic resistance in Streptococcus is becoming more worrisome and can be influenced by various factors such as:
-
heightened resistance to antibiotics
-
young age
-
isolation from the upper respiratory tract
-
hospitalization
-
residence in an urban area
-
daycare attendance
Choosing the Appropriate Antibiotic
Due to its effectiveness in targeting the bacteria that cause these diseases, penicillin is the drug of choice for most streptococcal infections. Its bactericidal action stems from its ability to inhibit the biosynthesis of cell-wall mucopeptides in the bacterial structure, ultimately leading to their destruction.
However, the use of penicillin for streptococcal infections may result in various adverse effects, primarily impacting the digestive system with manifestations such as nausea, diarrhea, and gastrointestinal discomfort. Furthermore, there exists a potential for severe allergic reactions, which, albeit less frequent, can be substantial and necessitate attention.
Resistance and Treatment Complications
The phenomenon of antibiotic resistance in streptococcal infections refers to the ability of streptococcus bacteria to survive and multiply despite antibiotic treatment, creating a significant challenge for treatment efficacy. The development of antibiotic resistance in Streptococcus bacteria can occur through the acquisition of resistance genes, such as erm(B) and erm(TR) genes.
These genes enable the bacteria to produce methylases that neutralize the effects of antibiotics, especially macrolides like erythromycin and azithromycin.
Preventing the Spread of Streptococcal Infections

A critical aspect of managing streptococcal conditions is preventing their spread. Regular and thorough hand washing is crucial for preventing the transmission of streptococcal infections. It is important to wash hands frequently, particularly after coughing or sneezing, before meals, and after using the restroom.
Hygiene and Wound Care
Effective handwashing methods include:
-
Wetting hands with clean water
-
Creating a soap lather
-
Scrubbing hands front and back, in between fingers, and under fingernails for at least 20 seconds
-
Thoroughly rinsing with clean water
-
Drying with a clean towel or air drying
To effectively prevent streptococcal infections, it is important to:
-
Regularly wash your hands
-
Use hand sanitizer
-
Practice proper sneezing and coughing etiquette to minimize the dissemination of infected respiratory droplets
By following these measures, you can lower the likelihood of transmitting the infection to others.
Vaccination and Public Health Measures
Despite their underutilization, pneumococcal vaccines have shown initial effectiveness and safety, winning approval in various countries, including the United States. Other streptococci still have vaccines that are in the experimental stage, indicating that further research and development is necessary..
On the other hand, the principal guidelines for pneumococcal vaccination in high-risk populations involve vaccination for:
-
all infants and children below 2 years of age
-
all adults aged 65 or above
-
adults with risk factors for pneumococcal disease or severe adverse outcomes
-
immunocompromised individuals
-
adult cigarette smokers aged 19 through 64 years.
Living with Post-Streptococcal Conditions
Conditions commonly occurring post-streptococcal infection include:
-
Acute rheumatic fever
-
Poststreptococcal reactive arthritis
-
Pediatric autoimmune neuropsychiatric disorders
-
Post-streptococcal glomerulonephritis
These conditions have the potential to result in enduring effects, including chronic kidney disease stemming from post-streptococcal glomerulonephritis.
It is therefore important to understand how to manage these chronic effects and monitor for potential complications.
Managing Chronic Effects
The management of chronic kidney disease resulting from post-streptococcal glomerulonephritis entails:
-
Controlling symptoms and preventing additional kidney damage
-
Implementing dietary adjustments such as restricting salt and water intake
-
Using prescribed diuretics
-
Managing high blood pressure
-
Monitoring protein levels in urine
-
Receiving ongoing care from a kidney specialist.
Additionally, through regular screenings, it facilitates proactive management to slow or halt kidney disease progression, thereby preventing kidney damage.
Monitoring for Complications
To ensure appropriate evaluation and management of any complications, patients with a history of streptococcal infection should follow their healthcare provider’s advice regarding medical check-ups. Potential complications resulting from untreated streptococcal infections encompass ear and skin infections, and in rare instances, life-threatening complications.
Tests such as the Strep A test, blood tests, throat cultures, and rapid antigen detection testing are conducted to monitor for complications of streptococcal infections.
Summary
Streptococcus is a group of bacteria that has a significant impact on human health, causing a range of illnesses from mild to severe. Early detection and appropriate treatment are crucial in managing these infections. Prevention measures such as maintaining good hygiene, proper wound care, and vaccination can help control the spread of these infections. Managing chronic effects and monitoring for complications are essential for individuals who have experienced streptococcal infections. As we continue to learn more about Streptococcus, we can improve our strategies for prevention, diagnosis, and treatment, ultimately improving health outcomes for those affected by these bacteria.
Frequently Asked Questions
How do you get a streptococcal infection?
Streptococcal infections are caused by Group A Streptococcus (GAS) bacteria, which can be transmitted through respiratory droplets from coughing or sneezing, as well as through direct contact with infected skin or surfaces. It is also spread through shared food or drinks and can be picked up from contaminated surfaces.
What is the most common disease caused by Streptococcus?
The most common disease caused by Streptococcus is throat infection (pharyngitis), followed by tonsil infection (tonsillitis), scarlet fever, skin sores (impetigo), and skin infection (cellulitis). Serious, potentially life-threatening infections are rare but can occur (iGAS).
What does Streptococcus do in the body?
Streptococcus can cause skin, soft tissue, and respiratory tract infections by spreading through respiratory droplets and contaminated surfaces. It is a type of bacteria that can lead to various infections.
What are the most common symptoms of streptococcal infections?
The most common symptoms of streptococcal infections are sore throat, difficulty swallowing, headache, fever, red and swollen tonsils, white patches on the tonsils, and swollen lymph nodes in the neck. If you experience these symptoms, it's important to seek medical attention promptly.
How are streptococcal infections diagnosed?
Streptococcal infections are diagnosed through various laboratory tests such as the bacitracin test, Lancefield antigen A test, and throat culture. Rapid antigen detection testing and the ASO test are also used for diagnosis.
Original content from the Upbility writing team. Reproduction of this article, in whole or in part, without credit to the publisher is prohibited.
You can also read:
- The Link Between ADHD and Exercise
- Improve Your Child's Self-Esteem With Extracurricular Activities
- ADHD and Lying: The Reasons Why Kids With ADHD Are Prone to Lying
- Back to School: Making it Easier for Students With Learning Disabilities
- ADHD and Substance Abuse in Teenagers A Research
- 5 Tips For A Happy Summer For Kids With ADHD
- The Impacts Of Distance Learning A Review
Suggested Books on ADHD:









